
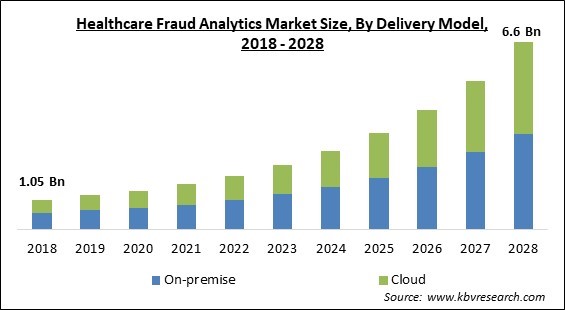
The Global Healthcare Fraud Analytics Market size is expected to reach $6.6 Billion by 2028, rising at a market growth of 23.0% CAGR during the forecast period.
Health-care fraud is characterized as illegal deception aimed at gaining financial benefit in the areas of medication manufacture, product quality, medical practice, and healthcare insurance. The practice of healthcare fraud includes cheating government-sponsored healthcare schemes, as well as defrauding insurance companies, businesses, and consumers. Leading life sciences companies are currently using a variety of data mining techniques to combat these fraudulent operations. These data mining techniques entail scouring databases for new information, such as healthcare insurance data, fraud strategies, and healthcare information systems, among other things.
In the coming years, the healthcare fraud detection market is expected to be driven by a rise in the number of fraudulent events in health care, an uptick in the frequency of patients going to opt for health care insurance, and an increase in the pressure to keep a record of fraud and abuse in health care spending. Other factors include a growth in the frequency of health care BPO and fraud identity management software, quick acceptance of cloud-based analytical solutions, increased influence of social media on the health care industry, and the efficiency of artificial intelligence in healthcare services & solutions.
With a unique visualization interface that allows users to go over individual and account views to evaluate all relevant activities and relationships at a network dimension, users may discover linkages within apparently unrelated claims. With social network diagrams and extensive data mining skills, organizations may gain an improved understanding of new dangers and prevent large losses before they happen. Additionally, by constantly developing models and modifying the system, organizations can keep in front of variations in payment and cost-cutting trends.
The healthcare fraud analytics industry is confronted with numerous obstacles. Business dynamics are being impacted by travel restrictions and quarantines, shuts down in outdoor/indoor activities, temporary business outages, supply-demand fluctuations, stock market volatility, diminishing business confidence, and a myriad of other worries. In the healthcare industry, doctors, patients, physicians, and other medical experts have all been engaged in fraud situations. Many healthcare professionals and experts have been discovered scamming patients for monetary gain. Patients' fraudulent acts in the healthcare sector include fraudulently obtaining sickness certificates, prescription fraud, and evasion of medical payments.
The number of people who have benefited from various healthcare initiatives has increased dramatically over time. The increase in the ageing population, growth in healthcare costs, and rising illness load are all factors leading to the expansion of the health insurance market. The number of people without health insurance in the United States has declined dramatically, from the year 2010 to the year 2016. During the 2017 open enrollment period, multiple millions of people signed up for or renewed their health insurance, as per National Center for Health Statistics.
The healthcare business is evolving at a breakneck pace, and one of the primary factors driving this evolution is the increasing influence of healthcare communication via social media. Not only has social media grown in popularity as a source of health information, but it also allows for dual-way public communication among patients, other third parties, and providers. This contributes to the creation of a big forum for comprehensive health discussions.
The execution of fraud analytics solutions consumes a huge time. Developing new databases, user interfaces, and predictive models; assessing and implementing models; and tracking their efficacy are all part of the process. During this step, data analysts execute algorithms till they find the best accurate forecasting model. The eave-droppers are very clever to notice that which organization is lacking regular upgrades & updates and is the deployment process time-consuming and accordingly plan & execute the unauthorized interference.
Based on delivery model, the healthcare fraud analytics market is bifurcated into On-premises and Cloud-based. The On-premises segment acquired the highest revenue share in the healthcare fraud analytics market in 2021. The simplicity of access to data being on-site, i.e., hospitals, etc., results in better record management and data monitoring, among other things. Current systems in small businesses are functional, but when scaled up, data management can become complicated and cumbersome, especially if the company is dealing with a large data set. This could imply a significant financial investment in data storage and security.
Based on Application, the healthcare fraud analytics market is divided into Insurance Claim Review, Pharmacy billing Issues, Payment Integrity, and Others. The pharmacy billing issue segment garnered a significant revenue share in the healthcare fraud analytics market in 2021. The increased frequency of medical billing fraud is happening in pharmacies. The objective of pharmacy billing is to reduce expenses from the admin side.
Based on end-use, the healthcare fraud analytics market is classified into Public & Government Agencies, Private Insurance Payers, Third-party Service Providers, and Employers. The Public & Government Agencies segment acquired the highest revenue share in the healthcare fraud analytics market in 2021. A greater amount of patients in government hospitals, as well as the increased vulnerability of government organizations to fraudulent operations because of a lack of technologically updated infrastructure, specifically in developing countries, are two significant factors leading to the big percentage.
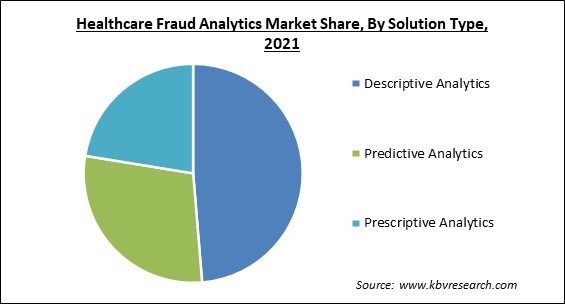
Based on solution type, the healthcare fraud analytics market is segmented into Descriptive Analytics, Prescriptive Analytics, and Predictive Analytics. The descriptive analytics segment acquired the highest revenue share in the healthcare fraud analytics market in 2021. For the purpose of identifying patterns and linkages, it uses both current and historical data. This aids in the more accurate detection of potential scams. It also serves as a foundation for implementing predictive and prescriptive analytics effectively. This contributes to the segment's continued expansion.
| Report Attribute | Details |
|---|---|
| Market size value in 2021 | USD 1.6 Billion |
| Market size forecast in 2028 | USD 6.6 Billion |
| Base Year | 2021 |
| Historical Period | 2018 to 2020 |
| Forecast Period | 2022 to 2028 |
| Revenue Growth Rate | CAGR of 23% from 2022 to 2028 |
| Number of Pages | 269 |
| Number of Tables | 450 |
| Report coverage | Market Trends, Revenue Estimation and Forecast, Segmentation Analysis, Regional and Country Breakdown, Competitive Landscape, Companies Strategic Developments, Company Profiling |
| Segments covered | Delivery Model, Application, Solution Type, End User, Region |
| Country scope | US, Canada, Mexico, Germany, UK, France, Russia, Spain, Italy, China, Japan, India, South Korea, Singapore, Malaysia, Brazil, Argentina, UAE, Saudi Arabia, South Africa, Nigeria |
| Growth Drivers |
|
| Restraints |
|
Free Valuable Insights: Global Healthcare Fraud Analytics Market size to reach USD 6.6 Billion by 2028
The leading players in the market are competing with diverse innovative offerings to remain competitive in the market. The below illustration shows the percentage of revenue shared by some of the leading companies in the market. The leading players of the market are adopting various strategies in order to cater demand coming from the different industries. The key developmental strategies in the market are Acquisitions, and Partnerships & Collaborations.
The market research report covers the analysis of key stake holders of the market. Key companies profiled in the report include Wipro Limited, IBM Corporation, DXC Technology Company, SAS Institute, Inc., Conduent, Incorporated, HCL Technologies Ltd., UnitedHealth Group, Inc. (Optum, Inc.), OSP Labs, Cotiviti, Inc., and ExlService Holdings, Inc.
By Delivery Model
By Application
By End User
By Solution Type
By Geography
The healthcare fraud analytics market size is projected to reach USD 6.6 Billion by 2028.
Growth In frequency of people looking for health insurance are increasing are driving the market in coming years, however, time-consuming deployment and the need for frequent upgrades growth of the market.
IBM Corporation, DXC Technology Company, SAS Institute, Inc., Conduent, Incorporated, HCL Technologies Ltd., UnitedHealth Group, Inc. (Optum, Inc.), OSP Labs, Cotiviti, Inc., and ExlService Holdings, Inc.
The Insurance Claim Review segment acquired maximum revenue share in the Global Healthcare Fraud Analytics Market by Application in 2021, and would continue to be a dominant market till 2028.
The Predictive Analytics market has the high growth rate of 23.3% during (2022 - 2028).
The North America market dominated the Global Healthcare Fraud Analytics Market by Region in 2021, and would continue to be a dominant market till 2028.
Our team of dedicated experts can provide you with attractive expansion opportunities for your business.
