The North America AI In Revenue Cycle Management Market would witness market growth of 23.3% CAGR during the forecast period (2025-2032).
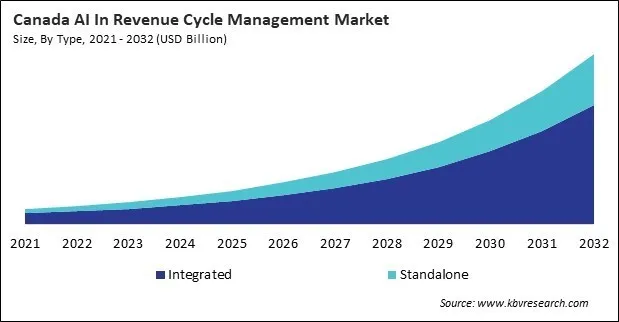
The US market dominated the North America AI In Revenue Cycle Management Market by Country in 2024, and would continue to be a dominant market till 2032; thereby, achieving a market value of $39,704.5 Million by 2032. The Canada market is experiencing a CAGR of 26% during (2025 - 2032). Additionally, The Mexico market would exhibit a CAGR of 24.9% during (2025 - 2032).
Artificial Intelligence (AI) has rapidly emerged as a transformative force across various sectors of the global economy, with the healthcare industry experiencing particularly profound change. Among the critical domains within healthcare, Revenue Cycle Management (RCM) stands out as an area where AI’s potential to drive efficiency, accuracy, and financial sustainability is increasingly evident. The integration of AI into RCM is reshaping how healthcare providers, payers, and associated stakeholders manage the complex web of administrative and financial processes required to track patient care episodes, from registration and appointment scheduling to final payment of a balance.
Revenue Cycle Management encompasses the comprehensive process of capturing, managing, and collecting patient service revenue, a cycle that begins at the time a patient schedules an appointment and concludes when the healthcare provider receives full payment for services rendered. Traditionally, RCM has been fraught with challenges, including manual data entry errors, fragmented workflows, claim denials, coding inaccuracies, delayed payments, and regulatory compliance complexities.
The United States is the world’s leading market for artificial intelligence in revenue cycle management, owing to its vast and complex healthcare ecosystem. The U.S. healthcare sector encompasses thousands of hospitals, clinics, payers, and physician groups, all operating under a multi-payer insurance model with a heavy administrative load. Rising healthcare costs, frequent coding updates, and mounting regulatory pressures have made the adoption of AI-powered RCM solutions a top priority for providers seeking to improve both profitability and patient care.
Canada’s publicly funded healthcare system is increasingly turning to artificial intelligence in revenue cycle management to address operational inefficiencies and meet rising expectations for service delivery. The country’s universal health coverage model, while eliminating the complexities of multi-payer billing, still faces challenges related to resource allocation, administrative burdens, and the integration of disparate provincial healthcare systems.
Mexico’s healthcare system is marked by a mix of public and private providers, with significant variation in quality, efficiency, and financial management across the sector. In recent years, the adoption of artificial intelligence in revenue cycle management has begun to accelerate as hospitals, insurers, and clinics recognize the benefits of automation in reducing administrative burdens and improving revenue collection.
Free Valuable Insights: The AI In Revenue Cycle Management Market is Predict to reach USD 107.17 Billion by 2032, at a CAGR of 23.7%
Based on Type, the market is segmented into Integrated and Standalone. Based on Delivery Mode, the market is segmented into Cloud-based, Web-based, and On-premise. Based on End Use, the market is segmented into Physician Back Offices, Hospitals, Diagnostic Laboratories, and Other End Use. Based on Application, the market is segmented into Claims Management, Medical Coding & Charge Capture, Financial Analytics & KPI Monitoring, Payment Posting & Remittance, and Other Application. Based on Product, the market is segmented into Software and Services. Based on countries, the market is segmented into U.S., Mexico, Canada, and Rest of North America.
By Type
By Delivery Mode
By End Use
By Application
By Product
By Country
Our team of dedicated experts can provide you with attractive expansion opportunities for your business.